Standing on the shoulders of giants: how a genetic discovery at SickKids in 1993 continues to inform research and patient care
Summary:
This month marks the 25th anniversary of the discovery of the gene responsible for Wilson disease by scientists at The Hospital for Sick Children (SickKids).
If I have seen further than others, it is by standing upon the shoulders of giants.
– Sir Isaac Newton
This month marks the 25th anniversary of the discovery of the gene responsible for Wilson disease by scientists at The Hospital for Sick Children (SickKids). The key paper, co-authored by Dr. Diane Cox, Principal Investigator, was published in the December 1993 edition of Nature Genetics. (See the initial coverage in The Globe and Mail (PDF) and in this 1994 SickKids publication (PDF) as well.)
Wilson disease (WD) is a rare metabolic disorder that impacts how the body handles copper, which is vital for human survival, and results in buildup of copper deposits in the liver, brain, cornea and other tissues. It affects approximately 1 in 30,000 people; there are an estimated 1,000 individuals in Canada living with WD.

Cox, a geneticist, joined SickKids after being recruited by Drs. Bibudhendra (Amu) Sarkar and Andrew Sass-Kortsak, as they were both interested in understanding the disease mechanism of Wilson disease. “We started writing grants together for our Wilson disease project,” says Sarkar. “The part belonging to the Wilson disease gene discovery was Diane’s own independent work within our group. Finding a gene in those days was difficult and extremely time-consuming work. But Diane persevered through all that and finally discovered the gene. She used Andrew’s patient materials for her work.”
Wilson disease was already known to be autosomal recessive, which means both parents have to pass down an affected chromosome. Therefore, there is a 25 per cent chance of each of their children having the disease, a 50 per cent chance of being a carrier, and 25 per cent chance of not being affected at all.
Cox’s team found that WD is due to mutations in the gene which encodes a protein that transfers copper across membranes within cells. The gene is named ATP7B. (The protein encoded in ATP7B was expressed, isolated and characterized in the Sarkar laboratory at SickKids by various biophysical techniques. They discovered the protein binds to copper for transport out of the body and identified the structures of all the binding sites.)

Dr. Eve Roberts, a paediatric hepatologist at SickKids who provided clinical care for WD patients for 23 years and is currently an Associate Fellow in the History of Science and Technology Program, University of King’s College, Halifax, was on Cox’s team that identified the gene. She had collaborated with Cox previously and was the only hepatologist on staff at the time. “Once you have the gene, you know what the gene product looks like in cells,” says Roberts. “You study the protein and what it interacts with, and you can target interaction with drugs. Now that we have the gene identified, we can consider gene repair.”
Roberts, who is also Adjunct Professor of Paediatrics, Medicine and Pharmacology & Toxicology, University of Toronto, co-authors the American Association for the Study of Liver Diseases’ internationally accepted guideline for clinical management of WD, and has co-edited a book released in September this year that covers bringing research findings on WD to caring for WD patients. She describes the ability to test genetically for WD as a “source of comfort” for patients, as it can present differently: as a neurologically caused condition such as tremors, as liver disease, and in almost 20 per cent of cases, as psychiatric disease. The genetic test is the only definitive diagnosis.
Shivam, 14, is an example of a WD patient at SickKids who was diagnosed via genetic testing as a result of an unrelated concern that ended up presenting as liver disease. In preschool, he was hyper and had a hard time paying attention. When the teacher mentioned this to his parents, they took him to the paediatrician, trying to find a root cause for his challenging behaviour. His bloodwork showed that his blood levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), enzymes that show liver damage or disease, were elevated.
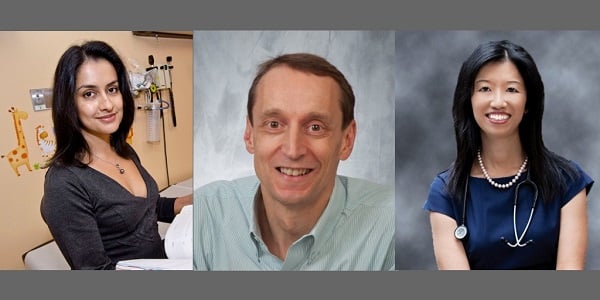
A patient getting lab work done to check liver enzymes for another reason (in this case, Shivam’s behaviour) is one of the three ways that WD patients come to be diagnosed, says Dr. Binita Kamath, one of three paediatric hepatologists at the Liver Clinic of the Division of Gastroenterology, Hepatology and Nutrition at SickKids, alongside Dr. Simon Ling and Dr. Vicky Ng. “In these cases, once the physician finds the enzymes to be elevated, the patient is sent to the Liver Clinic for a diagnosis through various tests, ending with a genetic screening if necessary.”
Once a child is diagnosed, biologically related siblings and other immediate family members are screened, which is the second way that patients come to be diagnosed. In Shivam’s case, this meant his fraternal twin Soham was also tested and subsequently diagnosed. Both boys were started on treatment, even though Soham was not showing any symptoms or concerning behaviours. Notably, while Shivam’s behaviour led to a WD diagnosis, the behaviour was not caused by WD; further testing indicated that he falls on the autism spectrum.

The final type of diagnosis occurs once patients are already showing signs and symptoms of WD, such as liver disease. “If we can offer early treatment before development of symptoms, this offers the best outcome,” says Roberts. If a patient has extremely advanced liver disease, the only path to survival is a liver transplant. Yet this isn’t common at SickKids, says Kamath: “We perform maybe one transplant a year for Wilson disease. In general we are able to treat patients medically, and this is quite successful.”
“Without a diagnosis and treatment, 99 out of 100 patients will die,” says Roberts. “But if you are diagnosed and put on meds and tolerate them and take them consistently, plenty of studies show that life expectancy could be over 70 years.”
Since starting in the 1960s to help children with liver disorders, the Liver Clinic at SickKids has treated over 80 children with WD. Currently and collectively, Drs. Kamath, Ling and Ng see around 20 WD patients. Kamath and Roberts are currently investigating acute liver failure due to WD and have several additional factors to consider.
Many of the patients seen in the clinic are new immigrants to Canada, especially from South Asia (India, Pakistan) and Syria. “Research publications on WD out of Europe are massively biased towards a Caucasian population, generalized to all populations,” says Kamath, “but at SickKids, the pattern of disease, its severity and its age of onset varies significantly among patients of different ethnic origins.”
Also of interest to Kamath and Roberts is “how even individuals in the same family can have very different patterns of the disease,” says Roberts. “How can some have it and some not? They are all in the same environment, have the same genetic change. Why does it manifest at different ages – four, 14, or 64? This is a clinical observation we have now and need to explain better.”

This is illustrated in Shivam and Soham’s family. The boys are the only ones with WD; their sister and their parents are carriers. But between the two boys, their disease has developed differently. After initial diagnosis, they were both put on a chelation agent called trientine that helps the body flesh out excess copper. They received this treatment for several years, and then were transitioned to a zinc salt for maintenance for another three years. Just last year, however, Soham’s ALT level was increasing and he needed to start on a chelation agent again, while Shivam showed no concerning changes in his bloodwork and continues on maintenance.
While Soham and his family await blood test results to determine the next course of action for treating and managing his disease, they continue to be grateful for the care they receive at SickKids and from the Liver Clinic specifically. “The doctor, the clinic, everyone at SickKids is excellent,” says his dad Manish. “The kids get excited to come to SickKids. We even brought a visiting cousin from India to the clinic to show them around!”
Clinicians and scientists from SickKids and beyond are working together on Wilson disease, building on the work of Cox’s team. “The discovery of the gene in 1993 allowed for certain diagnosis for our patients and for us to start treatment sooner,” says Roberts. “Now, with the discovery of the gene and 25 years of research, we are poised to look at epigenetics and at the gene and protein environment broadly, and how these might play a role in the differences we see in various populations and among family members. These research findings will continue to translate into better care for our patients.”

